Currently Empty: $0.00
Chronic Care Management (CCM), Principal Care Management (PCM) and Remote Physiologic Monitoring (RPM) have become essential tools for medical practices seeking to improve patient outcomes, expand access to care beyond the traditional office visit and create sustainable, value-aligned revenue streams. However, despite their potential, many practices struggle with implementation due to unclear operational requirements, inconsistent workflows, documentation gaps and heightened payer scrutiny.
This in-depth, practice-focused webinar is designed to help providers and practice leaders understand what must be in place before launching CCM, PCM and RPM services to ensure long-term success. Rather than focusing solely on billing opportunities, this session emphasizes the critical clinical, operational and compliance foundations that support these programs and protect practices from denials, recoupments and audit risk.
Attendees will gain clarity on patient eligibility, consent requirements, staffing and supervision models, technology selection and care coordination workflows necessary to deliver these services effectively at the provider office level. The session will also explore how to align care management activities with CMS guidance, ensure documentation supports billed services and establish internal oversight processes to maintain program integrity as volume grows.
Whether your practice is evaluating these services for the first time or looking to optimize an existing program, this webinar provides actionable best practices and real-world insights to help you confidently implement CCM, PCM and RPM in a compliant, scalable and patient-centered way.
Learning Outcomes:
By the end of this session, participants will be able to:
- Differentiate CCM, PCM and RPM services
- Understand the clinical intent, patient eligibility and use cases for each program
- Identify when CCM vs. PCM is most appropriate for a patient population
- Identify operational readiness requirements
- Assess staffing, workflows and care team roles required for successful implementation
- Understand provider, clinical staff and third-party vendor responsibilities
- Apply billing, coding and documentation best practices
- Review key CPT codes, time thresholds and supervision requirements
- Recognize common billing and documentation errors that trigger denials and audits
- Implement compliant patient enrollment and consent processes
- Understand CMS consent requirements and how to operationalize them
- Ensure ongoing patient engagement and documentation support
- Evaluate technology and vendor considerations
- Identify critical features practices should require from CCM/PCM/RPM platforms
- Understand data integration, reporting and audit support expectations
- Mitigate compliance and audit risk
- Align workflows with CMS guidance and payer scrutiny
- Establish internal monitoring and quality oversight processes
Areas Covered in the Session:
- Overview of CCM, PCM and RPM services and their clinical intent
- Patient eligibility criteria and appropriate program selection
- Practice readiness assessment and pre-implementation requirements
- Patient enrollment and CMS consent requirements
- Staffing models, care team roles and supervision expectations
- Care coordination workflows and patient engagement strategies
- Billing, coding and documentation essentials
- Common compliance risks, denials and audit triggers
- Technology and vendor selection considerations
- Participants will leave with a clear roadmap for implementing CCM, PCM and RPM services confidently while balancing patient care, operational efficiency, and compliance so these programs become a sustainable asset rather than an administrative burden
- Live Q&A Session
Recommended participants:
- Healthcare Executives & Leadership
- CEOs, COOs, CIOs, CISOs
- Practice administrators and hospital executives responsible for risk and compliance
- Compliance, Privacy & Risk Professionals
- HIPAA Compliance Officers
- Privacy Officers
- Risk management and governance professionals
- IT & Cybersecurity Teams
- Security architects and engineers
- SOC analysts and incident response teams
- Network, cloud and infrastructure engineers
- Healthcare IT Management
- IT directors and managers
- EHR/EMR systems administrators
- Health IT operations leaders
- Cloud & DevOps Professionals
- Cloud security engineers (AWS, Azure, GCP)
- DevSecOps and platform engineering teams supporting healthcare workloads
- Clinical & Operational Leaders
- Clinical informatics leaders
- Department heads involved in patient data workflows
- Telehealth and digital health program managers
- Legal & Audit Teams
- Healthcare legal counsel
- Internal and external auditors
- Third-party risk and vendor management teams
- Business Associates & Vendors
- Managed Service Providers (MSPs)
- Healthcare SaaS providers
- Medical device and digital health vendors handling ePHI
- Incident Response & Crisis Management Teams
- Business continuity and disaster recovery planners
- Emergency preparedness coordinators
- Healthcare Startups & Innovators
- Founders and product leaders building HIPAA-regulated solutions
- AI, data analytics and digital health innovators
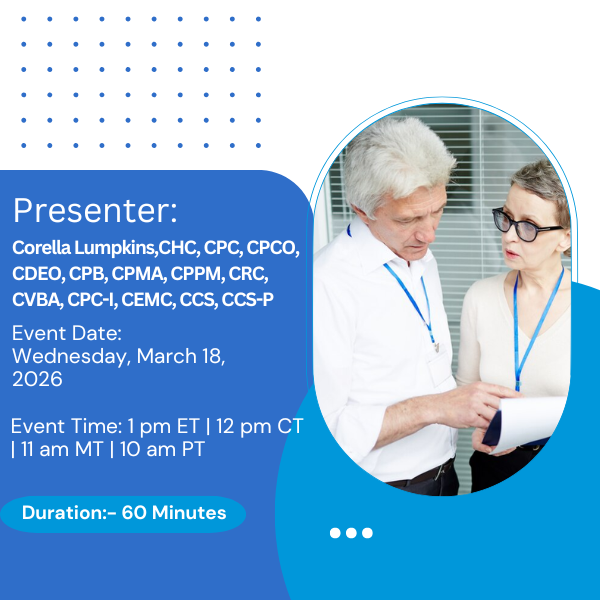
Presenter Biography:

Corella Lumpkins is Manager of Coding, Compliance and Provider education at Loudoun Medical Group (LMG), a physician-owned multi-specialty Accountable Care Organization in the Northern Virginia/DC suburbs. Corella works closely with providers in navigating patient-centric value-based care.
As a subject matter expert, she has over 36 years of experience working in every area of the healthcare revenue cycle on both the payer and provider sides. Corella holds a bachelor’s degree in healthcare administration, 13 certifications and has an extensive background in auditing, billing, coding, claims adjudication, implementing corporate compliance programs, CDI, education, risk adjustment, denials and practice management.
Corella has held leadership roles at GW, Lifebridge, Johns Hopkins and the University of Maryland health systems. Corella is a national speaker, published author, AAPC approved instructor, adjunct faculty for Towson University and the AAPC’s Emerging Leaders Program. She proudly serves an Education Officer for her local AAPC chapter, as a member of the 2025-2026 Association of Clinical Documentation Integrity Specialists (ACDIS) Leadership Council and as an Officer and committee chair for the 2025-2027 AAPC National Advisory Board.
Additional Information:
After registration, You will receive an email with login information and handouts (presentation slides) that you can print and share with all participants at your location.
System Requirement:
- Internet Speed: Preferably above 1 MBPS
- Headset: Any decent headset and microphone which can be used to talk and hear clearly
Can’t Listen Live?
No problem. You can get access to an On-Demand webinar. Use it as a training tool at your convenience. For more information, you can reach out to the below contact:
Toll-Free No: +1 800-757-9502
Email: cs@waymoreeducation.com