Currently Empty: $0.00
Payers don’t want you to know how much control you really have regarding your claims’ reimbursement. They don’t want you to know that by applying ERISA regulations, you can force your payers to:
- Pay your claims more quickly
- Stop downcoding your office visits
- Overturn claims that were previously denied
- Expand inadequate appeal deadlines
- Return recouped funds previously taken from your practice
Payers know that approximately 83% of your non-Medicare/Medicaid claims are governed by ERISA regulations. For these claims, insurance companies also know that their timely filing deadlines of 90-120 days don’t apply, that they can’t legally recoup funds you’ve been paid and that in most cases, your claims can’t be downcoded without your input. However, they do it anyway because no one is pushing back.
Well, if you are tired to feeling like payers are holding all the cards, David Zetter, CHC, CPCO, CPC, COC, PCS, FCS, CHBC, CMUP, PESC, CMAP, CMAPA, CMMP, CMHP, can help. David is going to break down the complexities of ERISA regulations into plain English. He’ll walk you through only the pieces you need, and then provide you with actionable advice on how to use it.
By attending this 90-minutes online training, you’ll learn how to utilize the applicable portions of ERISA regulations to have more control of your payer requirements and reimbursements. If you’ve experienced even one of the scenarios below, and want to “push back” to change futures outcomes, this online training is for you:
- Without warning, the payer takes back reimbursement from your future claims.
- Your claim is downloaded with no request for progress notes or doctor review.
- Your claim is refused because it arrived past the payer’s timely filing period.
- Your reimbursement is reduced because the payer bundled your services.
- Your payment is sent to the patient by mistake, and you’re expected to collect from them.
- Your appeal is denied because it reaches the payer past their 90-day deadline.
- Your claim is downcoded and the payer refuses to tell you why, or who authorized it.
- Your claim is denied for “investigational or experimental” services.
- You’re told to comply with state-balance billing laws when federal ERISA rules apply.
- You are denied assignment of benefits for being a non-contracted provider.
Payers are counting on the fact that only about 10% of practices really understand how to apply ERISA regulations to their claims. They don’t want you to know that ERISA regulations provide you with more control when it comes to how, when and what you are reimbursed for your services.
The bottom line is that by mastering the complexities of ERISA, you can significantly increase your reimbursement, and reduce the number of hoops that payers require you to jump through to get paid. Don’t wait, sign up for this online training today.
Learning Outcomes:
- What is a summary plan description and why is this or the policy the most important document you should have in your practice?
- Why so many do not know or understand the law and why you should?
- What ERISA protects and how it will help your practice?
- Which claims are covered by ERISA and which are not?
- What to do when you have an insurance company tell you what to do and it is against ERISA laws?
- Who’s claim is it?
Areas Covered in the Session:
- What is ERISA?
- Who Does ERISA Affect?
- When is it an ERISA Claim?
- ERISA Claims
- Not ERISA Claims
- Where ERISA Does Not Apply
- DOL & EBSA
- ERISA Time Limits
- Oversight of Health Benefit Plan
- What is a Fiduciary?
- What Gives You The Right?
- Assignment of Benefits
- Valid Assignment of Benefits
- ERISA Requirements
- Plan Document Requirements
- Summary Plan Description Requirements
- More About ERISA
- Provider Agreement V. Patient Policy
- Insurance Contracts
- Carrier Lies
- When they lie
- Laws: Don’t They Matter?
- What is an ABD?
- Advance Benefit Determination
- Most Powerful Documents
- Summary Plan Description
- Patient Health Insurance Policy
- What is a Summary Plan Description?
- Why you should obtain SPDs or Policies from Patients?
- Group Health Plans
- Reasonable Opportunity
- Full and Fair Review
- Communications with insurance Carrier
- ERISA and How to use it
- Medical Necessity ABDs
- Investigational/ Experimental Procedures
- Recouping on claims
- State Balance Billing Laws
- What about Bundling?
- What about Down-coding?
- Out of Network/ Non- Par
- Retroactive Benefit Denial
- PCA V. BCBSA
- Typical Violations of ERISA
- Penalties and Punishments
- Letter: Example
Recommended participants:
- Healthcare CEOs
- Healthcare CFOs
- Healthcare COOs
- Office managers
- Administrators
- Billing staff and companies
- Physicians and other providers
- Healthcare consultants
- Compliance Officers
- Physicians
- Nurses
- Practice Manager
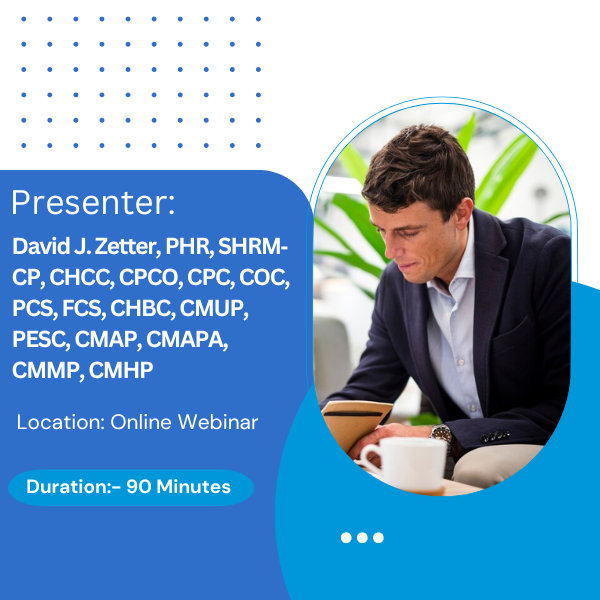
Presenter Biography:

David J. Zetter, PHR, SHRM‐CP, CHCC, CPCO, CPC, COC, PCS, FCS, CHBC, CMUP, PESC, CMAP, CMAPA, CMMP, CMHP, is the founder and President of Zetter HealthCare, LLC in Mechanicsburg, PA and has over 30 years of operational and healthcare experience. David is nationally recognized for his presentations and expertise. He is well-versed in regulatory requirements, revenue cycle management, credentialing and contracting, compliance, coding and documentation. He is considered an expert on Medicare, not only by his clients but his consultant colleagues across the country. He has evaluated existing ambulatory care facilities and practices with respect to patient flow, operations, marketing, fee structures, use of ancillary services and financial considerations; developing strategic plans to improve profitability and productivity. His activities in management and compliance include physician practices, IDTFs, hospitals, ASCs, pharmacy, DME and other facility types, including coding and broad‐based regulatory issues. David has also conducted chart audits on behalf of Medicare contractors and Blue Cross/Blue Shield early in his career, so he has knowledge of what the expectations are from the payers. David’s firm works with healthcare professional clients and facilities coast to coast, in all areas of practice and facility management including start‐ups, buy‐ins, compensation, exit strategies, reimbursement enhancement, practice financial modeling, governance documentation, policy and procedure development and implementation, credentialing and contracting, human resources staffing and management, compliance, coding and chart reviews, physician education and many other areas. David has helped to maximize both profitability and reimbursement of physician practices, facility and ambulatory practices, re‐engineered operational and human resources, and addressed coding and billing issues for providers to curtail fraud, abuse, kickback, OIG, and IRS issues. He is also an original member of CMS’ PECOS Power User Group, CMS Compliance Focus Group and MIPS Design Lean Work Group which provides feedback and recommendations to Medicare’s Center for Program Integrity and Provider Enrollment Operations Group on design and improvements to the PECOS enrollment environment, as well as, NPPES and MIPS and conducts beta testing of the EHR/HITECH user interfaces and environments at the request of the Office of e‐Health Standards & Services Director. David is also on the CMS contracted team awarded the PECOS 2.0 contract to rebuild PECOS from the ground up. David has conducted practice management, human resource, coding and compliance education and seminars in many states over the past twenty‐five years. David speaks often on a variety of practice management subjects at hospital residency programs, the National Society for Certified Healthcare Business Consultants, the Medical Management Group Association, the American Academy of Professional Coders, AHIMA, Florida Institute of Certified Public Accountants, Florida Medical Society, many other venues and is often called upon by the MGMA, HFMA, DecisionHealth, Part B News, Part B Insider, and many others, to conduct audio conferences and webinars. He has been published in Medical Economics and interviewed and quoted in many publications including Report on Patient Privacy and Report on Medicare Compliance.
Additional Information:
System Requirement:
- Internet Speed: Preferably above 1 MBPS
- Headset: Any decent headset and microphone which can be used to hear clearly
Can’t Listen Live?
No problem. You can get access to an On-Demand webinar. Use it as a training tool at your convenience. For more information, you can reach out to the below contact: Toll-Free No: +1 800-757-9502 Email: cs@waymoreeducation.com